Mastering Best Practices for Hemostat Safety
- lenoxinstro
- November 27, 2024
- Dental Forceps, Dental Instruments, Dental Surgical
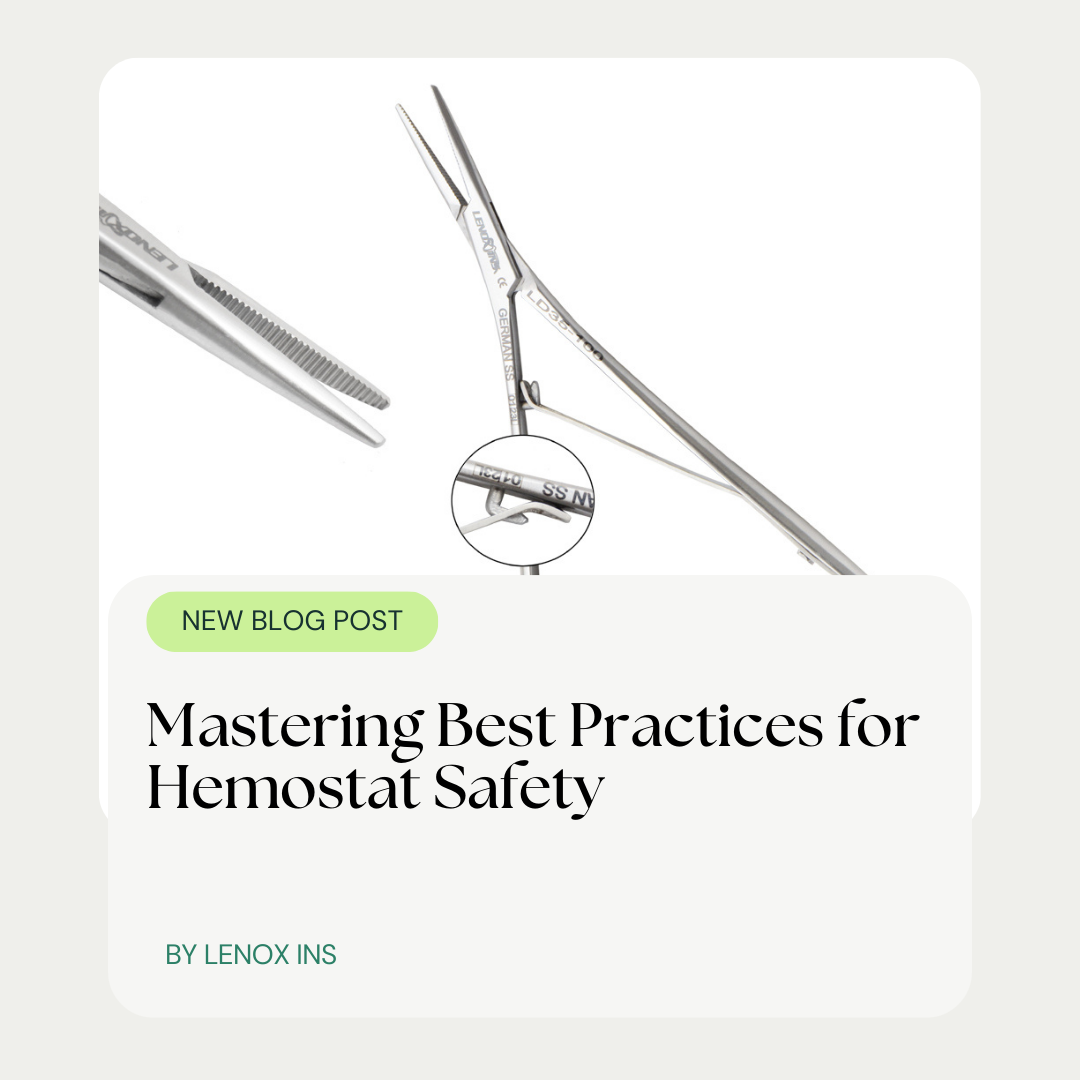
Did you know that using the wrong type of hemostat can lead to complications in surgical procedures? Ensuring the correct grip on blood vessels requires precise selection and handling of surgical tools like the Crile hemostat or the delicate mosquito variant. This article delves into the essentials of selecting the right hemostat, preparing it for use, and mastering its handling to maintain a safe surgical environment. By learning these best practices, you’ll enhance the longevity of your tools, like the indispensable scalpel and hemostat, while safeguarding against contamination. Equip yourself with the knowledge to make informed decisions and handle every situation with confidence.
Understanding Different Hemostat Types and Their Proper Uses
In medical procedures, the proper selection and application of hemostats are crucial. From Rochester Pean forceps to Kelly forceps and needle holders, each tool is designed for specific tasks. By identifying common hemostat types and recognizing their particular uses, healthcare professionals can ensure precision and safety during surgeries. This section delves into the characteristics of these instruments, all forged from resilient steel, and guides on their appropriate uses in various medical settings.
Identifying Common Hemostat Types in Medical Procedures
In the arena of surgical procedures, accurate identification and application of hemostat forceps are vital for effective hemostasis. For instance, a curved hemostat is commonly used in deeper or more confined spaces to grasp a blood vessel securely, while ensuring minimal tissue damage. Professionals must prioritize familiarity with these tools to guarantee a proper ligature and prevent inadvertent tissue trauma during surgeries.
It’s essential for surgical practitioners to harness the capabilities of various hemostat types to manage bleeding or suture sites effectively. The precision handling of a surgical suture can be dramatically improved with the use of the right hemostat forcep, enabling controlled compression and a stable working environment. Mastery of these instruments not only contributes to successful surgical outcomes but also heightens patient safety during operations.
Recognizing Specific Applications for Each Hemostat Type
Each hemostat type is crafted with precision to meet the demands of different surgical scenarios. For instance, Halsted mosquito forceps feature delicate jaws, making them ideal for gripping small vessels and executing fine, controlled movements. Scissors-like surgical forceps, on the other hand, are designed to enable quick and efficient cutting while maintaining a strong grip on tissues, succinctly illustrating the importance of tool specificity in medical practice.
In the dynamic environment of an operating room, understanding the nuances of each forceps becomes imperative. The alignment of the jaws, the pressure exerted by the handle, and the locking mechanism of a hemostat such as the Kelly forceps can significantly impact the outcome of a procedure. By recognizing these specific applications and handling nuances, surgical teams can minimize complications and enhance patient care.
Choosing the Appropriate Hemostat for Safe Surgical Procedures
Selecting the right surgical hemostats, such as curved Kelly forceps with a precise ratchet mechanism, is critical for the success of any surgery. Assessing patient needs is paramount in choosing hemostats that ensure secure blood vessel clamping and patient safety. Upcoming sections will delve into evaluating hemostat features for optimal performance during surgical procedures, offering healthcare professionals insight into making informed decisions for effective surgical outcomes.
Assessing Patient Needs to Select the Right Hemostat
When it comes to surgical precision, assessing patient needs is paramount in the selection process of hemostats. Considerations such as the patient’s vessel size and exposure area influence whether a mosquito hemostat or a broader retractor will be employed. Stainless steel mosquito forceps may be the instrument of choice for delicate procedures, due to their fine tips and precise control, which are essential for minimizing tissue damage and ensuring patient safety.
The diverse array of stainless steel hemostats serves different functions, from fishing out foreign bodies to clamping blood vessels. Surgeons assess the surgical site’s accessibility and the required clamping strength when deciding between a firm grip mosquito hemostat or a larger retractor. This decision-making process is critical to prevent postoperative complications and to ensure that the chosen hemostat aligns with the specific needs of each procedure and patient.
Evaluating Hemostat Features for Optimal Performance
When choosing a surgical instrument like a Kelly hemostat, health professionals must evaluate features such as the jaw configuration and locking mechanism, which are pivotal in managing tissue and controlling bleeding. A hemostat that aligns well with the tissue‘s structure can provide a secure clamp, reducing the risk of damage and ensuring that surgical goals are precisely met.
Further, proper assessment of hemostats and forceps involves understanding the balance and tactile feedback they provide, as these elements influence the surgeon’s ability to react swiftly to changes in the surgical field. Surgical teams prioritize instruments that offer a comfortable grip and controlled performance, which are essential for maintaining hemostasis throughout the procedure.
Preparing Hemostats Correctly for Safe and Effective Use
Proper preparation of surgical instruments, such as mosquito forceps curved, is essential for ensuring their safe and effective use during medical procedures. Before surgery, thorough inspection for any damage and strict adherence to sterility protocols are imperative steps. These practices help to maintain the functional integrity of hemostats and prevent postoperative infections. In the upcoming sections, we will explore the critical processes of inspecting hemostats and ensuring their sterility, which are key to upholding high standards of patient care and surgical success.
Inspecting Hemostats Thoroughly for Damage Before Procedures
Before the commencement of any procedure, it is essential for surgical teams to conduct a detailed inspection of hemostats for signs of wear or damage. Even minor imperfections in the instrument’s alignment or serration can compromise its grip on blood vessels, risking patient safety. This precautionary scrutiny helps avert the possibility of equipment failure, safeguarding the trajectory of the operation.
Professionals in the medical field understand that the integrity of a hemostat is fundamental to its function. They carefully examine each instrument for issues such as weakened locking mechanisms or blunt edges, which could lead to slippage or inadequate clamping during critical moments of surgery. Ensuring that each hemostat is in optimum condition is a key safety protocol that underscores the meticulous nature of surgical care.
Ensuring Sterility of Hemostats Prior to Procedures
Ensuring the sterility of hemostats is non-negotiable before their introduction into the surgical field. Surgical teams engage in rigorous sterilization processes, often involving autoclaving, to eradicate any microorganisms that could cause infection. This critical step underscores the relentless commitment to patient safety and the prevention of postoperative complications.
Sterilization protocols for hemostats must be meticulous, with attention to the integrity of the instrument after the process. Healthcare providers must verify that the high temperatures and pressures used during autoclaving have not compromised the hemostat‘s structure or function. Such diligence in preparing for surgery protects the well-being of patients and is a central part of operating room best practices.
Implementing Proper Handling Techniques for Hemostat Safety
Mastering the use of hemostats is pivotal in surgical practice to ensure patient safety and procedure efficacy. Accurately grasping the hemostat is fundamental to preventing slippage, while applying the correct amount of pressure is key to avoiding tissue damage. Upcoming discussions will provide healthcare professionals with essential tactics for handling hemostats, ensuring that each clinical intervention is as safe and efficient as possible.
Grasping the Hemostat Correctly to Prevent Slippage
Proper technique when grasping hemostats is critical to prevent slipping and maintain control. Surgeons are advised to hold the instrument firmly near the pivot point, a practice allowing for precise manipulation and reduced hand fatigue. This ensures sustained accuracy and stability when clamping vessels or tissues, directly influencing the success of a surgical procedure.
Consistent and competent handling of hemostats also involves recognizing the tactile cues provided by the instrument. When a surgeon feels the resistance as the hemostat locks in place, they can adjust their grip accordingly, mitigating the risk of slippage and unintended tissue damage. Such attentiveness to detail during hemostat handling is essential for upholding patient safety and achieving positive surgical outcomes.
Applying Appropriate Pressure to Avoid Tissue Damage
Surgical acumen demands the application of just the right amount of pressure when using hemostats, ensuring that blood vessels are secured without being crushed. Skilled surgeons gauge this with finesse, applying firm yet gentle pressure that prevents both slippage and the compromising of vascular integrity. Their proficiency in modulating force is crucial, helping to avoid tissue damage and ensuring a smooth recovery for patients.
Key to minimizing trauma to tissue during procedures, the calibrated use of hemostats speaks to the surgeon’s precision and care. A firm, yet careful closure of the hemostat‘s handles can achieve the delicate balance between maintaining hemostasis and preserving tissue. This practice is integral to patient outcomes, confirming yet again the importance of nuanced surgical technique in healthcare settings.
Cleaning and Sterilizing Hemostats to Prevent Contamination
The integrity of hemostats hinges not only on their construction but also on meticulous cleaning and sterilization. The immediate thorough cleaning of hemostats after use is indispensable, as it ensures the removal of biological debris to prevent contamination. Following best practice guidelines for sterilizing these precise tools is equally critical. Upcoming discussions will detail the essential steps and protocols that medical professionals must follow to maintain the cleanliness and function of hemostats, thereby upholding the highest standards of patient safety. These best practices offer actionable insights into the preparation of hemostats for repeat use, ensuring their safe integration into medical procedures.
Cleaning Hemostats Thoroughly Immediately After Use
Immediate cleaning of hemostats post-procedure is imperative to prevent the risk of cross-contamination. Healthcare professionals take care to remove all blood, tissue, and other biological materials, which, if left unchecked, can harbor bacteria and compromise the effectiveness of the sterilization process. This initial cleaning is a critical first step in ensuring that each hemostat remains hygienic and safe for subsequent use.
After each surgical application, the meticulous cleaning of hemostats typifies the diligence required to uphold safety standards. Utilizing appropriate cleaning solutions and techniques, medical staff work to ensure that no residual debris remains. Such thoroughness lays the groundwork for the sterilization phase, setting the stage for reliable disinfection and the preservation of the tools’ integrity.
Sterilizing Hemostats Following Best Practice Guidelines
Sterilization of hemostats adheres to strict guidelines to ensure that these critical surgical tools are free from microorganisms and safe for patient use. The process often involves autoclaving, where hemostats are subjected to high-pressure steam at a specific temperature for a set duration, a protocol outlined by healthcare regulatory bodies. Proper adherence to these sterilization standards is non-negotiable, as it directly impacts the asepsis of the surgical environment and patient health outcomes.
After the rigorous cleaning process, hemostats are packaged and placed in an autoclave, with careful attention to manufacturer instructions to preserve the integrity of the instruments. Healthcare professionals recognize that consistent monitoring of sterilization cycles and regular maintenance of the autoclave equipment are essential for optimal performance. By following these established protocols, medical teams demonstrate a commitment to excellence in patient care and uphold the reputation of their practice.
Maintaining Hemostats: Best Practices for Longevity and Safety
Ensuring the longevity and safety of hemostats hinges on performing regular maintenance checks and adopting proper storage methods. Regular examinations guarantee their precision and functional integrity, while correct storage conditions help extend their working life. This subsection illuminates the best practices for maintaining hemostats, detailing necessary routine checks and optimal storage techniques to preserve these essential surgical tools.
Performing Regular Maintenance Checks on Hemostats
Regular maintenance checks of hemostats are indispensable to ensure their optimal functionality and safety. Surgical teams perform these checks to uncover any issues with the instrument’s alignment, locking mechanisms, or jaw integrity, which could potentially jeopardize a procedure’s success. By proactively identifying and addressing wear and tear, healthcare providers maintain the high standards required for surgical instruments and patient care.
During these inspections, medical professionals take into account the smooth operation of the ratchet mechanism and the precision of the hemostat‘s teeth, confirming that they interlock correctly. Maintaining these crucial aspects of the instrument facilitates reliable performance in the operating room, where precise control and secure grasping of tissues are paramount for successful surgical outcomes.
Storing Hemostats Properly to Extend Their Lifespan
Proper storage of hemostats is essential in preserving their functionality and extending their operation life. These precision instruments should be kept in a dry, clean environment where temperatures are regulated to prevent corrosion and other damage. By housing them in designated areas with protective casings or organizers, medical facilities help ensure the tools remain in top condition, ready for the next procedure.
Careful attention to the positioning of hemostats during storage also plays a significant role in maintaining their lifespan. Ensuring that the instrument’s jaws and ratchet mechanism are not under undue stress while at rest can prevent misalignment and wear. Healthcare providers who prioritize these storage practices contribute significantly to the longevity and reliability of these indispensable surgical tools.
Conclusion
Effective hemostat safety and handling are paramount in surgical procedures, influencing patient outcomes and healthcare efficacy. Surgeons must meticulously select and apply the correct hemostats, ensuring their grasp and pressure are skillfully calibrated to prevent tissue damage. Rigorously cleaning, sterilizing, and maintaining these vital instruments not only prolong their usability but also safeguard against contamination, fostering a secure surgical environment. Ultimately, embracing these best practices is a testament to a medical team’s dedication to excellence in patient care and successful surgical interventions.